Piles Treatment
Piles and Fissure(GERD)
Piles (Haemorroids)
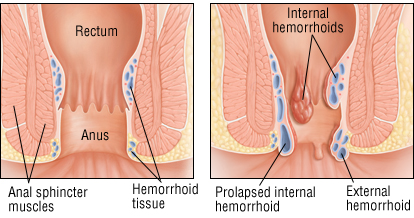
Haemorrhoids, also known as piles, are swellings that contain enlarged blood vessels that are found inside or around the bottom (the rectum and anus).
Most haemorrhoids are mild and sometimes don’t even cause symptoms. When there are symptoms, these usually include:
- Bleeding after passing a stool (the blood will be bright red)
- Itching around buttocks
a lump or swelling outside of the anus.
What causes piles(haemorrhoids) ?
Piles are associated with increased pressure in the blood vessels in and around your anus.
- Being overweight or obese
- Persistent constipation, often due to a lack of fibre in your diet
- Prolonged diarrhoea
- Regularly lifting heavy objects
- A persistent cough or repeated vomiting
- Prolonged sitting down
- Being pregnant (the haemorrhoids will usually improve after you give birth)
- Being over 45 years of age – as you get older, your body’s supporting tissues get weaker, increasing your risk of haemorrhoids
- A family history of haemorrhoids, which could mean you’re more likely to get them.
Symptoms of piles (Haemorrhoids)
They may include:
- Bleeding after passing a stool (the blood will be bright red)
- Itchiness around your anus
- A lump outside of the anus.
- A sticky, slimy (mucus) discharge after passing a stool
- Soreness, redness and swelling around your anus
Haemorrhoids are not usually painful, unless their blood supply slows down or is interrupted.
Preventing and treating piles
Haemorrhoids that occur due to pregnancy usually get better after child birth.
However, making lifestyle changes to reduce the strain on the blood vessels in and around your anus is often recommended. These include:
- Increasing the amount of fibre in your diet – good sources of fibre include fruit, green vegetables, wholegrain rice.
- Drinking plenty of fluid, particularly water 2.5 to 3 litres per day, but avoiding or cutting down on caffeine and alcohol
- Not delaying going to the toilet – ignoring the urge to empty your bowels can make your stools harder and drier, which can lead to straining when you do go to the toilet
- Avoiding medication that causes constipation
- Losing weight if you are overweight
- Exercising regularly – this can help prevent constipation, reduce your blood pressure and help you lose weight
These measures can also reduce the risk of haemorrhoids returning, or even developing in the first place.
Medication that you apply directly to your back passage (topical treatments) prescribed by your doctor may ease your symptoms and make it easier for you to pass stools.
If your haemorrhoid symptoms are more severe, there are a number of treatment options available.
Diagnosing piles (haemorrhoids)
Piles (haemorrhoids) can be easily diagnosed by your doctor. To do so, they will examine your back passage .
- Rectal examination
Your doctor may examine the outside of your anus to see if you have visible haemorrhoids, and they may also carry out an internal examination called a digital rectal examination (DRE). - Proctoscopy
In some cases, further internal examination using a proctoscope may be needed. A proctoscope is a thin hollow tube with a light on the end that is inserted into your anus. - Colonoscopy:
In some cases doctor may advice you Colonoscopy or endoscopy to rule out any other medical conditions like cancer or inflammatory bowel disease.
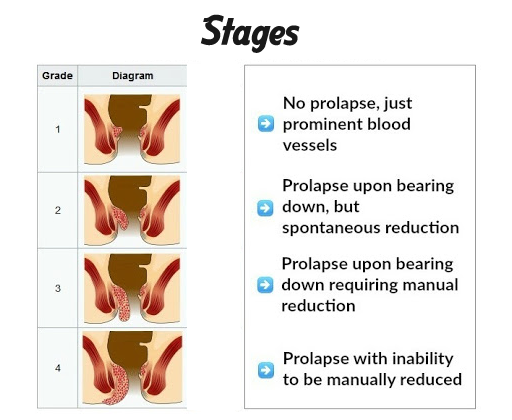
Grades of haemorrhoids
After a rectal examination or proctoscopy, your doctor can determine what type of haemorrhoid you have
- First Grade – small swellings that develop on the inside lining of the anus and are not visible from outside the anus
- Second Grade – larger swellings that may come out of your anus when you go to the toilet, before disappearing inside again
- Third Grade – one or more small soft lumps that hang down from the anus and can be pushed back inside (prolapsing and reducible)
- Fourth Grade – larger lumps that hang down from the anus and cannot be pushed back inside (irreducible)
It’s useful for doctors to know what type and size of haemorrhoid you have, as they can then decide on the best treatment.
Treating piles (haemorrhoids)
Lifestyle changes
However, making lifestyle changes to reduce the strain on the blood vessels in and around your anus is often recommended. These include:
- Increasing the amount of fibre in your diet – good sources of fibre include fruit, green vegetables, wholegrain rice.
- Drinking plenty of fluid, particularly water 2.5 to 3 litres per day, but avoiding or cutting down on caffeine and alcohol
- Not delaying going to the toilet – ignoring the urge to empty your bowels can make your stools harder and drier, which can lead to straining when you do go to the toilet
- Avoiding medication that causes constipation
- Losing weight if you are overweight
- Exercising regularly – this can help prevent constipation, reduce your blood pressure and help you lose weight
Medical Treatment
- Corticosteroid cream : If you have severe inflammation in and around your back passage, your doctor may prescribe corticosteroid cream, which contains steroids.
- Painkillers : Common painkilling medication, such as paracetamol, can relieve the pain of haemorrhoids. Products that contain local anaesthetic (painkilling medication) may also be prescribed by your doctor to treat painful haemorrhoids.
- Laxatives : Patients suffering from piles are usually constipated, doctor will prescribe a laxative. This will help you empty your bowels.
Non-surgical treatments
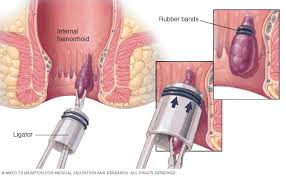
If dietary changes and medication don’t help, your doctor may recommend appropriate treatment non-surgical procedures such as banding and sclerotherapy this is usually done in Grade ! and Grade II piles
Banding
Banding is a procedure that involves placing a very tight elastic band around the base of your haemorrhoids, to cut off their blood supply. The haemorrhoids should then fall off within about a week of having the treatment. This procedure is done in out patient department and does not require anaesthesia
Injections (sclerotherapy)
A treatment called sclerotherapy may be used as an alternative to banding.
During sclerotherapy, a chemical solution is injected into the blood vessels in your back passage. This relieves pain by numbing the nerve endings at the site of the injection. It also hardens the tissue of the haemorrhoid so that a scar is formed. After about four to six weeks, the haemorrhoid should decrease in size.
Surgery for piles (haemorrhoids)
Surgery may be recommended if other treatments for piles (haemorrhoids) have not been successful, or if you have large haemorrhoids that are not suitable for non-surgical treatment.
There are many different surgical procedures for piles. The main types of operation are described below.
Haemorrhoidectomy
A haemorrhoidectomy is an operation to remove haemorrhoids. It is usually carried out under general anaesthetic or spinal anaesthesia.
After having a haemorrhoidectomy, there is around a 1 in 20 chance of the haemorrhoids returning, which is lower than with non-surgical treatments. Adopting or continuing a high-fibre diet after surgery is recommended to reduce this risk.
Transanal haemorrhoidal dearterialisation (THD) or haemorrhoidal artery ligation (HALO)
Transanal haemorrhoidal dearterialisation (THD) or haemorrhoidal artery ligation (HALO) is an operation to reduce the blood flow to your haemorrhoids.
It’s usually carried out under general anaesthetic and involves inserting a small device, which has a Doppler ultrasound probe attached, into your anus. This probe produces high-frequency sound waves that allow the surgeon to locate the blood vessels in and around your anal canal. These blood vessels supply blood to the haemorrhoid.
Stapler Heamorroidectomy:
Stapling, also known as stapled haemorrhoidopexy, is an alternative to a conventional haemorrhoidectomy. It is sometimes used to treat prolapsed haemorrhoids and is carried out under general anaesthetic. Post operative pain is less as compared to traditional operation.
General risks of haemorrhoid surgery
Although the risk of serious problems is small, complications can occasionally occur after haemorrhoid surgery. These can include:
- bleeding or passing blood clots
- infection, which may lead to a build-up of pus (an abscess).
- urinary retention (difficulty emptying your bladder)
Cost of Piles (Haemorroids) Surgery:
Cost depends on lots of factors such as
- Bed category
- Type of Surgery (stapled or haemorroidectomy)
- Preexisting medical conditions such as diabetes, angina which may prolong your hospital stay or need critical monitoring.
Following your first meeting with the doctor, we would be able to give you an approximate estimate.
MEDICAL TREATMENTS : NON-SURGICAL TREATMENTS
Banding
Banding is a treatment in which a very tight elastic band is wrapped around the base of your haemorrhoids to cut off their blood supply.
After the therapy, the haemorrhoids should come out within a week. This treatment is performed in the outpatient department and requires no anaesthesia.
Sclerotherapy (injections)

A treatment called sclerotherapy may be used as an alternative to banding. A chemical solution is injected into the blood vessels in your back passage during sclerotherapy. This relieves pain by numbing the nerve endings at the injection site. It also hardens the tissue of the haemorrhoid, resulting in the formation of a scar. The haemorrhoid should decrease in size after four to six weeks.
Laser
Haemorrhoid laser procedure (LHP) is a new laser method with promising outcomes for the treatment of haemorrhoids in which laser coagulation stops blood flow to the hemorrhoidal (piles) plexus. It is a day care technique with minimal pain that is performed under short anaesthesia
Fissure
What is an anal fissure?
An anal fissure is a tear or a small tear in the skin at the lower end of the anus (back passage). The condition is also referred to as Fissure-in-ano. It is due to pressure forced onto the wall of the anal canal either by the passage of hard stool or straining with a loose stool.
What are the symptoms?
- Pain : The pain is severe and sharp on and following bowel action and it can last a few minutes to several hours. The pain is caused by spasm of the anal sphincter (the inner circle of muscle in the anal canal). Because of the pain, patients with this condition fear bowel movement and often try to avoid it. This leads to further constipation with harder stools, which in turn increases the pain.
- Bleeding : The tear may result in bleeding during bowel movement.
- Skin tag : Sometimes swelling can occur near or around the fissure. This can cause a skin tag to develop (a piece of skin which hangs from surrounding skin).
- Mucus discharge (oozing) which causes
- Excoriation (rubbing of the area around) and itchiness around anus.
What are the Treatments?
Conservative (without surgery) treatment :
- High fibre diet By eating a high fibre diet you should aim to keep your stools soft but bulky.
- Increase fluids Drinking plenty of water (about 2 to 2.5 litres per day) will also help to keep your stools soft.
- Local anaesthetic ointment: Sometimes applying local anaesthetic ointment before and after a bowel movement makes passing stools easier with less pain. Your doctor may prescribe you an ointment to relieve spasm locally and to reduce swelling.
Surgical treatment:
If the above measures have not healed your fissure, surgery might be considered. The operation for anal fissure is called a lateral sphincterotomy and it has a high success rate of curing fissures.